“Official data have shown that the large-scale vaccinations undertaken in the US have failed to obtain any significant improvement of the diseases against which they were supposed to provide protection.” Dr A. Sabin, developer of the Oral Polio vaccine
Dr A. Sabin, developer of the Oral Polio vaccine (lecture to Italian doctors in Piacenza, Italy, December 7th 1985)
Subclinical Measles Occured In 45% of Vaccinated Children Exposed To Measles
‘Subclinical measles occurred in 45 percent of vaccinated children exposed to natural measles. “new epidemics, albeit milder in form, may occur in vaccinated areas[, a fact] which should be recognised in campaigns to eradicate measles.”
The Lancet, vol. 353, January 9, 1999, pp. 98-102.
A History Of Prior Vaccination Is Not Always Associated With Immunity
30 measles sufferer’s WITH detectable anti-bodies to measles were studied.
17 of these cases had been previously vaccinated against measles.
Clin. Invest. Med., vol. 11, no. 4, August 1988, pp. 304-9.
Measles outbreak in a fully immunized secondary-school population
An outbreak of measles occurred among adolescents in Corpus Christi, Texas, in the spring of 1985, even though vaccination requirements for school attendance had been thoroughly enforced. Serum samples from 1806 students at two secondary schools were obtained eight days after the onset of the first case. Only 4.1 percent of these students (74 of 1806) lacked detectable antibody to measles according to enzyme-linked immunosorbent assay, and more than 99 percent had records of vaccination with live measles vaccine. Stratified analysis showed that the number of doses of vaccine received was the most important predictor of antibody response. Ninety-five percent confidence intervals of seronegative rates were 0 to 3.3 percent for students who had received two prior doses of vaccine, as compared with 3.6 to 6.8 percent for students who had received only a single dose. After the survey, none of the 1732 seropositive students contracted measles. Fourteen of 74 seronegative students, all of whom had been vaccinated, contracted measles. In addition, three seronegative students seroconverted without experiencing any symptoms. We conclude that outbreaks of measles can occur in secondary schools, even when more than 99 percent of the students have been vaccinated and more than 95 percent are immune.
N Engl J Med 1987 Mar 26;316(13):771-4.
80% Of Children With Measles Had Been Vaccinated
Cases of measles among 165 vaccinated and unvaccinated children were studied and the level of measles antibody in 230 previously vaccinated children was determined. Associations between demographic factors and immunological response to vaccination were also investigated. Approximately 80% of the children with measles had been vaccinated; their cases had significantly lower rates of complication.
Measles Attack Rate Was Much Higher In Vaccinated Than Unvaccinated Children
Cherry et al. (1972) described an epidemic in St Loius Cityand County during 1970 & 1971, during which 130 children were hospitalised and 6 died. The attack rate was much higher in vaccinated than unvaccinated children.
J Pediatr 1973 May;82(5):802-8.
Measles inclusion-body encephalitis caused by the vaccine strain of measles virus – Measles Virus Found In Vaccinated Baby’s Brain
We report a case of measles inclusion-body encephalitis (MIBE) occurring in an apparently healthy 21-month-old boy 8.5 months after measles-mumps-rubella vaccination. He had no prior evidence of immune deficiency and no history of measles exposure or clinical disease. During hospitalization, a primary immunodeficiency characterized by a profoundly depressed CD8 cell count and dysgammaglobulinemia was demonstrated. A brain biopsy revealed histopathologic features consistent with MIBE, and measles antigens were detected by immunohistochemical staining. Electron microscopy revealed inclusions characteristic of paramyxovirus nucleocapsids within neurons, oligodendroglia, and astrocytes. The presence of measles virus in the brain tissue was confirmed by reverse transcription polymerase chain reaction. The nucleotide sequence in the nucleoprotein and fusion gene regions was identical to that of the Moraten and Schwarz vaccine strains; the fusion gene differed from known genotype A wild-type viruses.
Revue / Journal Title
Clinical infectious diseases ISSN 1058-4838 CODEN CIDIEL
Source / Source
Congrès
1999 Annual IDSA Meeting (1999)
1999, vol. 29, no 4, pp. 960-1112 (52 ref.), pp. 855-861.
Due to Vaccination Measles Now Affects Adults When It Is More Serious – 58% of Vaccinated People Had One Or More Symptoms Of Measles
An outbreak of measles at the University of California at Los Angeles provided the opportunity to study clinical, epidemiologic, and serologic characteristics of the disease in young adults in the present vaccine era. Of the 34 cases studied, 18 occurred in persons who thought they were immune. Fifteen of 19 seronegative students vaccinated during the epidemic responded with a secondary (IgG) antibody response. Antibody prevalence studies indicated that 91% of the student population had measles antibody at the onset of the outbreak, and history relating to measles correlated poorly with antibody prevalence. Of 212 adults vaccinated, 58% complained of one or more symptoms. Seventeen percent were confined to bed, and in three women vaccine-associated illness was notably severe. That measles will continue to be a problem in adults with our present national approach to immunization is predicted.
Ann Intern Med. 1979 Jun;90(6):873-6. PMID: 443682; UI: 79185850.
Outbreak Of Measles In Vaccinated Children In A Slum
Three cases of measles were admitted in Deptt. of Paediatrics, Govt. Medical College & Hospital, Chandigarh and were reported to the Deptt. of Community Medicine for an outbreak investigation. A trained team investigated the slum having a population of 25,000 and studied various features associated with epidemic between the period of April 22 to May 10, 2003. RESULTS: The study covered 484 houses having 1130 children. Among the children who developed measles 32.76% were vaccinated ones. In them attack rate was 3%. Attack rate in vaccinated children went on increasing as age increased. An overall attack rate of 5.13% (Peak incidence 6% in 1-4 years age group) was recorded. Among measles cases, one-fifth had post measles complications. As much as 32.76% children with measles had received measles vaccination in the past. Therefore something more than immunization by single dose of vaccine is required. Measles was reported to be higher amongst the children without Vitamin A supplementation (P<0.001). CONCLUSION: There is need to store vaccine properly and to strengthen routine immunization coverage, Vitamin A supplementation and health infrastructure in underprivileged population. Serological studies among vaccinated children against measles should be undertaken to explore the possibility of second dose of measles in older children.
Source: Indian Journal of Medical Sciences, 2004, vol.58, issue 2, p. 47-53.
VAN UK’S Comment: It’s interesting they mention vitamin A and underprivileged populations. Measles complications can be caused by vitamin A deficiency and they can be prevented by the administration of vitamin A. Pity they never tell parents.
Here’s What Happens When You Vaccinate Babies Against Measles – Measles Epidemic Now Hits Adults 18-40 As Vaccine Wanes. Measles Is Serious In Adults And There Are 10 People In Critical Condition
The measles epidemic has occurred in several northern provinces, targeting adults aged 18-40 instead of children as usual, according to epidemiologists.
The disease can develop quickly and serious after-effects can include damage to cognitive functions, experts said.
The National Hospital for Infectious and Tropical Diseases is treating about ten measles patients, who are in comas, and listed as in a critical condition.
The number of measles patients has risen by 20 times to reach nearly 250 since the discovery of the first case two months ago. Ninety percent of them come from Hanoi.
The patients had initial symptoms such as light temperature and rashes which first began in the ears and then spread to their heads, faces and the soles of their feet.
The Central Epidemiology Institute and the National Hospital for Infectious and Tropical Diseases are actively working together to identify cases of infection and guide clinics in provinces and cities to fight the disease.
The best way to prevent measles is to get vaccinated now and once again in the next 20 years, said Dr Nguyen Van Kinh, head of the hospital.
Source: VOV News, 4th February 2009.
VAN UK’S Comment: or how about letting your child have measles when they’re little and getting life-long immunity and protection from the severe complications of measles in adulthood?
Vaccine No Match Against Measles – Most Cases Had Been Vaccinated
Local health authorities have expressed concern about the rise in the number of persons in Lanao del Sur and Maguindanao suffering from measles even if they had been immunized.
Dr. Kadil Sinolinding, health secretary of the Autonomous Region in Muslim Mindanao said on Tuesday that at least 39 persons, aged eight months to 21 years old, were infected with measles in Lanao del Sur and Maguindanao.
The number of cases have been recorded since January but Sinolinding said the fact that most of those with measles had received anti-measles vaccines was “quite alarming.”
Sinolinding said that in the case of Maguindanao, many of the victims were evacuees from the ongoing conflict in Mindanao.
The good news, he said, was that no one had died of the viral infection – which could be fatal if complications arose.
“No fatality and all the patients have recovered,” Sinolinding told the Philippine Daily Inquirer.
He said the Department of Health has started investigating the cases to find out why patients, who had been immunized, still contracted the disease.
“We are trying to determine why despite the immunization, these patients still contacted the virus of measles,” Sinolinding said.
He said the immune systems of patients might have weakened over time due to some other factors.
He said the appalling conditions in evacuation centers might have weakened the people’s immune systems.
Source: Inquirer.net, 30th March 2010.
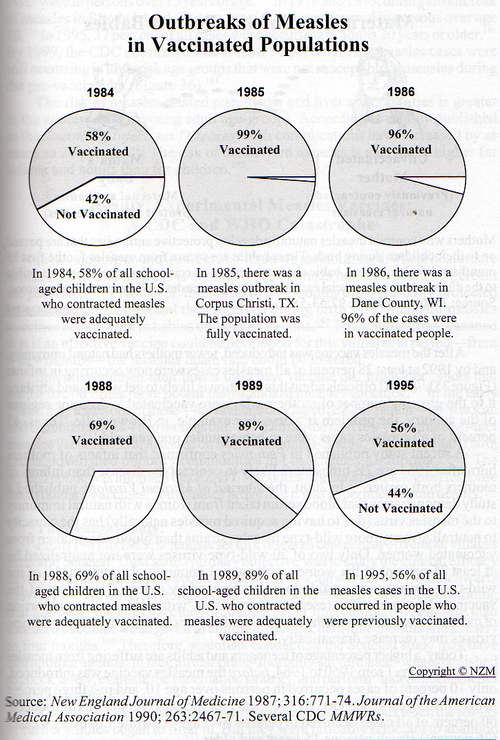
The Paradox of Measles Infections in Immunized Persons, Some Epidemics are in 100% Vaccinated People
Background
Measles is the most transmissible disease known to man. During the 1980s, the number of measles cases in the United States rose dramatically. Surprisingly, 20% to 40% of these cases occurred in persons who had been appropriately immunized against measles. In response, the United States adopted a two–dose universal measles immunization program. We critically examine the effect of vaccine failure in measles occurring in immunized persons.
Methods
We performed a computerized bibliographic literature search (National Library of Medicine) for all English-language articles dealing with measles outbreaks. We limited our search to reports of US and Canadian school-based outbreaks of measles, and we spoke with experts to get estimates of vaccine failure rates. In addition, we devised a hypothetical model of a school where measles immunization rates could be varied, vaccine failure rates could be calculated, and the percentage of measles cases occurring in immunized students could be determined.
Results
We found 18 reports of measles outbreaks in very highly immunized school populations where 71% to 99.8% of students were immunized against measles. Despite these high rates of immunization, 30% to 100% (mean, 77%) of all measles cases in these outbreaks occurred in previously immunized students. In our hypothetical school model, after more than 95% of schoolchildren are immunized against measles, the majority of measles cases occur in appropriately immunized children.
Conclusions
The apparent paradox is that as measles immunization rates rise to high levels in a population, measles becomes a disease of immunized persons. Because of the failure rate of the vaccine and the unique transmissibility of the measles virus, the currently available measles vaccine, used in a single-dose strategy, is unlikely to completely eliminate measles. The longterm success of a two-dose strategy to eliminate measles remains to be determined.
Source: Arch Intern Med. 1994;154:1815-1820. http://archinte.ama-assn.org/cgi/content/abstract/154/16/1815
Measles-vaccinated Israeli boy with subacute sclerosing panencephalitis.
Subacute sclerosing panencephalitis is a rare neurologic disorder of childhood and adolescence. We describe a 16-year-old boy who manifested the disease despite proper vaccinations. He was hospitalized because of bedwetting, involuntary limb movements, abnormal speech, and balance disturbances. Immunoglobulin G antibodies against measles were strongly positive, with a high relative cerebrospinal fluid/serum ratio. Polymerase chain reaction for measles produced negative results. Electroencephalography registered slow activity with high voltage discharges every few seconds, and with triphasic complex morphology. Magnetic resonance imaging revealed diffuse white matter changes, mostly around the posterior regions and lateral ventricles. Treatment with valproic acid, levetiracetam, carbamazepine, and intravenous immunoglobulin G was ineffective. Inosiplex and interferon-β-1a were also administrated. The patient became comatose, with generalized myoclonic jerks, and died 1 year later. An autopsy was not performed. This patient illustrates that subacute sclerosing panencephalitis should be suspected among young vaccinated subjects.
Source: Pediatr Neurol. 2011 Jun;44(6):467-70. http://www.ncbi.nlm.nih.gov/pubmed/21555060
Measles among vaccinated Quebec kids questioned – 50% of Cases were Vaccinated
An investigation into an outbreak in a high school in a town that was heavily hit by the virus found that about half of the cases were in teens who had received the recommended two doses of vaccine in childhood — in other words, teens whom authorities would have expected to have been protected from the measles virus.
It’s generally assumed that the measles vaccine, when given in a two-dose schedule in early childhood, should protect against measles infection about 99 per cent of the time. So the discovery that 52 of the 98 teens who caught measles were fully vaccinated came as a shock to the researchers who conducted the investigation.
“That’s the real question. How could that have happened?” said Dr. Gaston De Serres, an infectious diseases expert with Quebec’s public health agency and one of the authors of the study.
Source: CBC News, 20th October 2011.
Measles outbreak continues in Canada, even among immunized population (50% of Cases Vaccinated).
The measles outbreak in Canada continues to occur in both vaccinated and unvaccinated individuals and is causing concern over vaccine effectiveness, according to a presentation here during the IDSA 49th Annual Meeting.
“While this still ongoing outbreak feeds largely on unvaccinated individuals, the high proportion of cases who received two doses raises concerns on vaccine effectiveness,” Philippe Belanger, MSc, Ministère de la santé et des services sociaux du Québec, Montréal, told Infectious Diseases in Children. “However, the take-home message is still to get vaccinated.”
Source: Pediatric Supersite, 23rd October 2011.
11 Year Old Vaccinated Boy Dies of Rare Measles Complication
Then, about a month ago, doctors at Doernbecher Children’s Hospital at OHSU diagnosed it: Sean had Dawson Disease; a rare, neurological condition caused by the measles virus. Less than 10 people in the United States are reported to have it each year.
“He actually had the vaccine itself, the first dose, but it didn’t protect him,” Alpapara told KOIN. She says when Sean was a baby he got the measles virus in the Philippines, after he had been vaccinated. Alpapara says that often times, vaccines in other countries are not as strong as they are in the United States.
She thought when he had the measles and survived, that would be the worst of it.
“He almost died then. But I never thought there was some kind of disease that just laid dormant in his brain for 10 years,” she said.
Source: Koinlocal6, 17th February 2012.
30 Children in Wales Get Measles, All had One Dose of MMR
Thirty children have been diagnosed with measles at an outbreak connected to the Ysgol Eifionydd School in Porthmadog, North Wales.
Of the 30 children affected by the outbreak, none of them have received more than one dose of the MMR vaccine. Two doses of the vaccine are required to protect against measles, mumps and rubella.
Source: Vaccine News Daily, 2nd March 2012.
VAN UK’s Comment: Actually, the 2nd dose is only given to supposedly catch the 10% of people who fail to respond to the first vaccine, meaning that 90% of those vaccinated with one dose should still be ‘immunized’.
A Fully Vaccinated Woman Contracted And Then Spread the Measles Read more: http://www.smithsonianmag.com/smart-news/fully-vaccinated-woman-contracted-and-then-spread-measles
Get the measles vaccine, and you won’t get the measles—or give it to anyone else. Right? Well, not always. A person fully vaccinated against measles has contracted the disease and passed it on to others. The startling case study contradicts received wisdom about the vaccine and suggests that a recent swell of measles outbreaks in developed nations could mean more illnesses even among the vaccinated.
Less than 1% of people who get both shots will contract the potentially lethal skin and respiratory infection. And even if a fully vaccinated person does become infected—a rare situation known as “vaccine failure”—they weren’t thought to be contagious.
That’s why a fully vaccinated 22-year-old theater employee in New York City who developed the measles in 2011 was released without hospitalization or quarantine. But like Typhoid Mary, this patient turned out to be unwittingly contagious. Ultimately, she transmitted the measles to four other people, according to a recent report in Clinical Infectious Diseases that tracked symptoms in the 88 people with whom “Measles Mary” interacted while she was sick. Surprisingly, two of the secondary patients had been fully vaccinated. And although the other two had no record of receiving the vaccine, they both showed signs of previous measles exposure that should have conferred immunity.
A closer look at the blood samples taken during her treatment revealed how the immune defenses of Measles Mary broke down. As a first line of defense against the measles and other microbes, humans rely on a natural buttress of IgM antibodies. Like a wooden shield, they offer some protection from microbial assaults but aren’t impenetrable. The vaccine (or a case of the measles) prompts the body to supplement this primary buffer with a stronger armor of IgG antibodies, some of which are able to neutralize the measles virus so it can’t invade cells or spread to other patients. This secondary immune response was presumed to last for decades.
By analyzing her blood, the researchers found that Measles Mary mounted an IgM defense, as if she had never been vaccinated. Her blood also contained a potent arsenal of IgG antibodies, but a closer look revealed that none of these IgG antibodies were actually capable of neutralizing the measles virus. It seemed that her vaccine-given immunity had waned.
Although public health officials have assumed that measles immunity lasts forever, the case of Measles Mary highlights the reality that “the actual duration [of immunity] following infection or vaccination is unclear,” says Jennifer Rosen, who led the investigation as director of epidemiology and surveillance at the New York City Bureau of Immunization. The possibility of waning immunity is particularly worrisome as the virus surfaces in major U.S. hubs like Boston, Seattle, New York, and the Los Angeles area. Rosen doesn’t believe this single case merits a change in vaccination strategy—for example, giving adults booster shots—but she says that more regular surveillance to assess the strength of people’s measles immunity is warranted.
Source: Science Daily, 11th April 2014 – http://news.sciencemag.org/health/2014/04/measles-outbreak-traced-fully-vaccinated-patient-first-time
Outbreak of Measles Among Persons With Prior Evidence of Immunity, New York City, 2011
Background. Measles was eliminated in the United States through high vaccination coverage and a public health system able to rapidly respond to measles. Measles may occur among vaccinated individuals, but secondary transmission from such individuals has not been documented.
Methods. Suspected patients and contacts exposed during a measles outbreak in New York City in 2011 were investigated. Medical histories and immunization records were obtained. Cases were confirmed by detection of measles-specific immunoglobulin M and/or RNA. Tests for measles immunoglobulin G (IgG), IgG avidity, measurement of measles neutralizing antibody titers, and genotyping were performed to characterize the cases.
Results. The index patient had 2 doses of measles-containing vaccine; of 88 contacts, 4 secondary patients were confirmed who had either 2 doses of measles-containing vaccine or a past positive measles IgG antibody. All patients had laboratory confirmation of measles infection, clinical symptoms consistent with measles, and high-avidity IgG antibody characteristic of a secondary immune response. Neutralizing antibody titers of secondary patients reached >80 000 mIU/mL 3–4 days after rash onset and that of the index was <500 mIU/mL 9 days after rash onset. No additional cases of measles occurred among 231 contacts of secondary patients.
Conclusions. This is the first report of measles transmission from a twice-vaccinated individual with documented secondary vaccine failure. The clinical presentation and laboratory data of the index patient were typical of measles in a naive individual. Secondary patients had robust anamnestic antibody responses. No tertiary cases occurred despite numerous contacts. This outbreak underscores the need for thorough epidemiologic and laboratory investigation of suspected cases of measles regardless of vaccination status.
Source: Clin Infect Dis. (2014) 58 (9): 1205-1210.
http://cid.oxfordjournals.org/content/58/9/1205
VAN UK’s Comment: This report incorrectly states this is the first time a vaccinated person has spread the disease but this isn’t true. There are cases of epidemics in 100% vaccinated populations in medical literature. For instance, http://www.cdc.gov/mmwr/preview/mmwrhtml/00000359.htm
http://www.ncbi.nlm.nih.gov/pubmed/3821823
http://www.ncbi.nlm.nih.gov/pubmed/16322148
A measles outbreak at a college with a prematriculation immunization requirement.
Explosive School-based Measles Outbreak
Explosive School-based Measles Outbreak Intense Exposure May Have Resulted in High Risk, Even among Revaccinees
Even high levels of measles vaccination coverage have not always prevented outbreaks of measles spread by airborne transmission. It has been suggested that a large inoculum might increase vaccine failure risk. Airborne transmission might occasionally entail a large measles inoculum. The epidemiologic relevance of measles among properly vaccinated persons (i.e., those vaccinated after 15 months of age and with live attenuated virus) is increased when they become contagious. The authors studied inoculum intensities as measured by proxy variables and the contagiousness of properly vaccinated persons who contracted measles among 51 measles patients infected in one school, at home, or elsewhere, utilizing preexisting records of measles cases and 214 healthy controls from an explosive school outbreak that occurred in a rural Finnish municipality in 1989. One “super-spreader” infected 22 others in one day, including eight once-vaccinated students and one twice-vaccinated student, probably during an assembly of 144 students in a poorly ventilated hallway with no sunlight. Those infected later at home had high measles risk, even if they were revaccinees.
Full Text (PDF)
Source:
-
Am. J. Epidemiol. (1998) 148 (11): 1103-1110.
A measles outbreak at a college with a prematriculation immunization requirement.
BACKGROUND. In early 1988 an outbreak of 84 measles cases occurred at a college in Colorado in which over 98 percent of students had documentation of adequate measles immunity (physician diagnosed measles, receipt of live measles vaccine on or after the first birthday, or serologic evidence of immunity) due to an immunization requirement in effect since 1986. METHODS. To examine potential risk factors for measles vaccine failure, we conducted a retrospective cohort study among students living in campus dormitories using student health service vaccination records. RESULTS. Overall, 70 (83 percent) cases had been vaccinated at greater than or equal to 12 months of age. Students living in campus dormitories were at increased risk for measles compared to students living off-campus (RR = 3.0, 95% CI = 2.0, 4.7). Students vaccinated at 12-14 months of age were at increased risk compared to those vaccinated at greater than or equal to 15 months (RR = 3.1, 95% CI = 1.7, 5.7). Time since vaccination was not a risk factor for vaccine failure. Measles vaccine effectiveness was calculated to be 94% (95% CI = 86, 98) for vaccination at greater than or equal to 15 months. CONCLUSIONS. As in secondary schools, measles outbreaks can occur among highly vaccinated college populations. Implementation of recent recommendations to require two doses of measles vaccine for college entrants should help reduce measles outbreaks in college populations.
Source: Am J Public Health. 1991 March; 81(3): 360–364.
Lawrence Solomon: Vaccines can’t prevent measles outbreaks
Measles in highly immunized societies occurs primarily among those previously immunized.
The recent outbreaks of measles in Canada and the United States came as a shock to many public health experts but they wouldn’t have to Dr. Gregory Poland, one of the world’s most admired, most advanced thinkers in the field of vaccinology.
The measles vaccine has failed, he explained two years ago in a prescient paper, “The re-emergence of measles in developed countries.” In that paper, he warned that due to factors that most haven’t noticed, measles has come back to be a serious public health threat. Thankfully, in that paper and elsewhere he also spelled out in no-nonsense fashion what now needs to be done.
Dr. Poland is no vaccine denier. Not only is he among the harshest and most outspoken critics of the “irrationality of the antivaccinationists,” he is also one of the strongest proponents for vaccines and the good that they can do. As Professor of Medicine and founder and leader of Mayo Clinic’s Vaccine Research Group, one of the world’s largest vaccine research organizations; as editor-in-chief of the peer-reviewed scientific journal, Vaccine; as recipient of numerous awards; as chair of vaccine data monitoring committees for pharmaceutical giant Merck; as patent holder in various vaccines processes; as someone who enjoys special employee status with the Centers for Disease Control and the U.S. Department of Defense and as someone who has sat on every federal committee that has dealt with vaccines, no one can accuse him of seeing vaccines from a narrow perspective.
And he sees the need for a major rethink, after concluding that the current measles vaccine is unlikely to ever live up to the job expected of it: “outbreaks are occurring even in highly developed countries where vaccine access, public health infrastructure, and health literacy are not significant issues. This is unexpected and a worrisome harbinger — measles outbreaks are occurring where they are least expected,” he wrote in his 2012 paper, listing the “surprising numbers of cases occurring in persons who previously received one or even two documented doses of measles-containing vaccine.” During the 1989-1991 U.S. outbreaks, 20% to 40% of those affected had received one to two doses. In a 2011 outbreak in Canada, “over 50% of the 98 individuals had received two doses of measles vaccine.”
Source: Financial Post, 1st May 2014 – full article here: http://business.financialpost.com/2014/05/01/lawrence-solomon-vaccines-cant-prevent-measles-outbreaks/
Mom of 3-Year-Old Measles Patient Calls Diagnosis ‘Shocking’
The mother of a measles-infected child said she was shocked and scared when doctors gave her the diagnosis.
Kellie Krueger’s son Uriah is one of the at least 84 confirmed measles cases in a multi-state outbreak that started in December at Disneyland amusement park in California.
Krueger said she was surprised when doctors told her that her son had measles. Uriah was given one dose of the MMR vaccine that helps protect against the measles virus, but was too young to get the recommended second dose that would help further his protection.
“It was such a weird, old fashion thing like, ‘Who gets measles?'” Krueger said. “He had his vaccination, so it was a little bit shocking to find out that he had still gotten the measles.”
Source: ABC News, 31st January 2015, http://abcnews.go.com/Health/mom-year-measles-patient-calls-diagnosis-shocking/story?id=28630801
Measles transmission among adults with spread to children during an outbreak: Implications for measles elimination in China, 2014.
Abstract
INTRODUCTION:
Following implementation of China’s 2006-2012 Action Plan for measles elimination, which led to a nadir of measles in 2012, a resurgence started in 2013 that continued into 2014. Measles typically is a disease that mainly affects children. We investigated a community outbreak in 2014 with measles virus transmission among adults without children serving as virus reservoirs. Our investigation highlights adult susceptibility to measles.
METHODS:
We conducted a retrospective active case search, and analyzed confirmed case data to describe person, place, and time characteristics of the outbreak. All individuals with measles with onset during the first 2 months of the outbreak were interviewed face-to-face to determine source(s) of infection and transmission route (from whom and to whom).
RESULTS:
Among the 280 cases, 220 (77.6%) were among ≥20-year-old adults, 24 (8.6%) were among 8-23 month olds, 22 (7.9%) were among <8-month-old infants, and the remaining 14 (5.9%) were among 2-19 year olds. Of the 83 cases in the early stage of the outbreak, 41 (49.4%) were acquired in the community, 24 (28.9%) were acquired nosocomially, 13 (15.7%) were acquired by family contact, and 5 were imported. Among 44 clearly determined transmission linkages, 37 (84.1%) were adult to other age-group (these include 29 adult-to-adult, seven adult-to-child, and one adult-to-infant), six were from infants to adult and children, and one was child-to-child. Outbreak response immunization activities were implemented by non-selective supplementary immunization activities, with 51.3% of targeted 5-19-year-old children and adolescents, and 30.2% of targeted 20-49-year-old adults being vaccinated.
CONCLUSIONS:
Despite high population immunity among children and adolescents following three rounds of measles vaccine supplementary immunization activities, sustained measles virus transmission still occurred among adults in this community. Adult measles immunity gaps might threaten measles elimination, highlighting the importance targeting susceptible adults during outbreak response immunization.
Source: Vaccine. 2016 Jun 18. pii: S0264-410X(16)00232-2. doi: 10.1016/j.vaccine.2016.02.051. [Epub ahead of print]
http://www.ncbi.nlm.nih.gov/pubmed/27329182
[Measles outbreak in a Dutch region with high vaccination coverage].
Abstract
BACKGROUND:
Measles is one of the most contagious infectious diseases. One measles patient can infect 12 to 18 persons in a fully susceptible population, i.e. people who have not been vaccinated against or infected with measles. We describe a measles outbreak in a Dutch region with high vaccination coverage.
CASE DESCRIPTION:
After a visit from an Indian business partner, measles was confirmed in an Israeli employee of a medium-sized company in South Limburg. This initiated source and contact tracing by the local Public Health Services, leading to information and vaccination campaigns at the company and at the international school attended by the employee’s children. During the outbreak, three of the employee’s children and two colleagues also experienced measles. The diagnosis of measles in the Indian business partner was confirmed in the Netherlands based on the clinical symptoms.
CONCLUSION:
Laboratory confirmation of measles is important to allow timely source and contact tracing by the local Public Health Services. The work environment can play an important role in the spread of vaccine-preventable diseases.
Source: Ned Tijdschr Geneeskd. 2015;159:A8898.
http://www.ncbi.nlm.nih.gov/pubmed/26173663
Measles Virus Infection Among Vaccinated and Unvaccinated Children in Nigeria.
53.2% of Infected Girls and 56.8% of Boys Had Been Vaccinated and 39.7% were Unvaccinated
Abstract
This study investigated measles infection in vaccinated and unvaccinated children presenting with fever and maculopapular rash during measles outbreaks in the southern and western states of Nigeria. Measles, an acute viral illness caused by a virus in the family Paramyxoviridae, is a vaccine-preventable disease. Measles outbreak is common in Nigeria, despite the national immunization program. Children presenting with symptoms of measles infection in general hospitals and health centers in the states of southern and western Nigeria were recruited for this study. Vaccination history, clinical details, and 5 mL of blood were obtained from the children. Their sera samples were screened for specific immunoglobulin M antibodies to measles virus. Of 234 children tested (124 [53.2%] female), 133 (56.8%) had previously been vaccinated against measles virus, while 93 (39.7%) had not been vaccinated. Vaccination information for eight children could not be retrieved. One hundred and forty-three (62.4%) had measles IgM antibodies. Of these, 79 (55.3%) had been vaccinated for measles, while 65 (44.7%) had not. Despite the ongoing vaccination program in Nigeria, a high number of children are still being infected with measles, despite their vaccination status. Therefore, there is need to identify the reason for the low level of vaccine protection.
Source: Viral Immunol. 2015 Jul-Aug;28(6):304-8. doi: 10.1089/vim.2014.0118. Epub 2015 Jun 23.
http://www.ncbi.nlm.nih.gov/pubmed/26102341
Assessing the risk of measles resurgence in a highly vaccinated population: Belgium anno 2013.
Abstract
Despite long-standing two-dose measles-mumps-rubella (MMR) vaccination, measles outbreaks still occur in highly vaccinated European populations. For instance, large measles outbreaks occurred in France (2008–13), the United Kingdom (2012–13) and the Netherlands (2012). Based on a multicohort model approach, using spatial serological survey data, MMR vaccination coverage data and data on social contacts, we found effective reproduction numbers significantly higher than 1 for measles in Belgium. This indicates that at one of the expected re-introductions, a measles outbreak is likely to spread, especially when it occurs during school term. The predicted average effective reproduction number increased over a 30-year time span from 1.3 to 2.2 and from 1.9 to 3.2 for basic reproduction numbers of 12 and 18, respectively. The expected relative measles incidence was highest in infants under one year of age, in adolescents and young adults. In conclusion, gradually increasing proportions of susceptible adolescents and young adults provide through their highly active social life an avenue for measles to resurge in large outbreaks upon re-introduction in Belgium, especially during school terms. Infants form an important vulnerable group during future measles outbreaks.
Source: Euro Surveill. 2015 Jan 8;20(1). pii: 20998.
http://www.ncbi.nlm.nih.gov/pubmed/25613653
Measles Outbreak in a Highly Vaccinated Population – Israel, July-August 2017.
9 cases of measles occurred in a highly vaccinated population.
Source: MMWR Morb Mortal Wkly Rep. 2018 Oct 26;67(42):1186-1188. doi: 10.15585/mmwr.mm6742a4.
Outbreak of measles among persons with prior evidence of immunity, New York City, 2011.
Measles was eliminated in the United States through high vaccination coverage and a public health system able to rapidly respond to measles. Measles may occur among vaccinated individuals, but secondary transmission from such individuals has not been documented.
METHODS:
Suspected patients and contacts exposed during a measles outbreak in New York City in 2011 were investigated. Medical histories and immunization records were obtained. Cases were confirmed by detection of measles-specific immunoglobulin M and/or RNA. Tests for measles immunoglobulin G (IgG), IgG avidity, measurement of measles neutralizing antibody titers, and genotyping were performed to characterize the cases.
RESULTS:
The index patient had 2 doses of measles-containing vaccine; of 88 contacts, 4 secondary patients were confirmed who had either 2 doses of measles-containing vaccine or a past positive measles IgG antibody. All patients had laboratory confirmation of measles infection, clinical symptoms consistent with measles, and high-avidity IgG antibody characteristic of a secondary immune response. Neutralizing antibody titers of secondary patients reached >80 000 mIU/mL 3-4 days after rash onset and that of the index was <500 mIU/mL 9 days after rash onset. No additional cases of measles occurred among 231 contacts of secondary patients.
CONCLUSIONS:
This is the first report of measles transmission from a twice-vaccinated individual with documented secondary vaccine failure. The clinical presentation and laboratory data of the index patient were typical of measles in a naive individual. Secondary patients had robust anamnestic antibody responses. No tertiary cases occurred despite numerous contacts. This outbreak underscores the need for thorough epidemiologic and laboratory investigation of suspected cases of measles regardless of vaccination status.
Source: Clin Infect Dis. 2014 May;58(9):1205-10. doi: 10.1093/cid/ciu105. Epub 2014 Feb 27. https://www.ncbi.nlm.nih.gov/pubmed/24585562?fbclid=IwAR25XzmwRvnf13GuF_3nYNzsV3-EVsaiV-UlgC2iVQ_XwyjysVN8u2pvx90
An increasing, potentially measles-susceptible population over time after vaccination in Korea
Waning levels of measles antibodies with increasing time post-vaccination suggests that measles susceptibility is potentially increasing in Korea. This trend may be related to limitations of vaccine-induced immunity in the absence of natural boosting by the wild virus, compared to naturally acquired immunity triggered by measles infection. This study provides an important view into the current measles herd immunity in Korea.
Highlights
- •
-
Measles-specific antibodies wane in the absence of boosting by the wild-type virus.
- •
-
The number of potential measles-susceptible individuals progressively accumulates.
- •
-
Vaccine-induced immunity is less effective than naturally acquired immunity.
Source: https://doi.org/10.1016/j.vaccine.2017.06.058 https://www.sciencedirect.com/science/article/pii/S0264410X17308551?fbclid=IwAR0fLc1Sph2_ifcT0cSSI54Nc2pJXiMc-yYxIa4XT0T7EpTmR_J53Qq5LoQ
Spotlight on measles 2010: Excretion of vaccine strain measles virus in urine and pharyngeal secretions of a child with vaccine associated febrile rash illness, Croatia, March 2010
We describe excretion of measles vaccine strain Schwarz in a child who developed a febrile rash illness eight days after primary immunisation against measles, mumps and rubella. Throat swabs and urine specimens were collected on the fifth and sixth day of illness, respectively. Genotyping demonstrated measles vaccine strain Schwarz (genotype A). If measles and rubella were not under enhanced surveillance in Croatia, the case would have been either misreported as rubella or not recognised at all.
Source:

